What is Perimenopause, and Am I In It?
The Big Picture
Perimenopause is the transitional phase before menopause, marked by fluctuating hormones that gradually decline, though not always in a consistently straight line. This stage can cause symptoms including hot flashes, sleep disturbances, and changes in cognitive function, sexual function, and mood. Although it is a “natural” transition, this shift can bring about major discomfort, interruptions in your day-to-day function, and cause you to question your sanity.
What You Need to Know About Perimenopause
Perimenopause is deeply misunderstood by women themselves and broadly ignored by medical providers. This blog post aims to empower you to learn about the physical transitions your body goes through during perimenopause and equip you with strategies on how best to navigate this time of your life.
What is Perimenopause?
Perimenopause is the natural and normal period when your body adjusts to the end of your reproductive years. It’s also sometimes called the menopausal transition.
Menopause is often referred to as a point in time rather than a stage. You reach it exactly twelve consecutive months after you’ve had your last menstrual period, marking the definite end of your fertility. The average age of official menopause is 51, but symptoms leading up to being officially menopausal may come years earlier or persist years after.
How a woman experiences perimenopause is unique to the individual. How it feels, when it starts, and how long it lasts varies enormously from one woman to the next. Here are some generalities:
On average, perimenopausal symptoms begin in your mid-late-40s, but in some women, can start as early as late 30s or as late as early 50s.
Perimenopausal symptoms typically last around 4 years, but some unlucky women can persist for 10 or more.
The variety and severity of perimenopausal symptoms also differ widely among women.
Perimenopause and Hormones
Perimenopause is marked by the slow loss of both estrogen and progesterone.
Estrogen
Ovaries are the leading producers of estrogen, your primary female sex hormone, influencing nearly every organ and system in your body. The ovaries produce roughly the same amount of estrogen throughout your fertile years, but during perimenopause, they gradually produce less and less. That said, it is not a steady, predictable decline. Estrogen generally trends downward, but fluctuates dramatically along the way, rising and falling unevenly, sometimes dropping very low, other times spiking higher than usual. Eventually, in the later stages of perimenopause, estrogen production sinks, your ovaries no longer release eggs, and your periods cease.
Considering that your ovaries have been producing a steady supply of estrogen since adolescence, your body may begin to roller coaster. Menstrual cycles can become unpredictable, and you may experience physical and emotional symptoms. Systems that rely on estrogen may struggle to adjust. Estrogen affects:
Neurochemistry, modulates serotonin, gaba and dopamine, affecting mood (depression and anxiety) and mental clarity
Central nervous system, compromising sleep
Thermoregulatory, causing hot flashes and night sweats
Integumentary, affecting collagen synthesis, skin elasticity, thickness,and hydration
Metabolic system, affecting appetite (estrogen acts as an anorectic, suppressing appetite) and increasing adipose belly fat and reducing energy expenditure
Genitourinary system (vaginal dryness, UTI frequency)
Cardiovascular system (estrogen protects heart health)
Musculoskeletal system, reducing bone density
Progesterone
During perimenopause, progesterone declines before estrogen does. During perimenopause, women frequently have irregular ovulation, and ovulation is responsible for progesterone production. Even in cycles where ovulation occurs, the luteal phase (the second half of the cycle) is frequently shortened, giving the corpus luteum (which produces progesterone) an abbreviated time to function. In other words, ovarian aging is responsible for progesterone decline. Without progesterone to balance estrogen, perimenopausal (and postmenopausal) women may experience continued hormonal imbalances, contributing to symptoms such as anxiety, insomnia, and mood changes.
Progesterone affects:
Mood - loss of progesterone can cause increased anxiety, depressive symptoms, general mood instability
Sleep - progesterone helps with sleep onset, length and quality
Vasomotor symptoms - i.e., hot flashes and night sweats
Cycle irregularity - loss of progesterone contributes to irregular and often shorter, more frequent cycles
Integumentary, affecting collagen and thickness (not as impactful as estrogen)
Testosterone
Testosterone levels also decline with reproductive aging, although the significance of the decline varies among individuals.
Testosterone can affect:
Mood
Bone density
Weight
Sleep
Sexual function
Am I in Perimenopause?
You can think of perimenopause as your body going through estrogen and progesterone withdrawal. While some women don’t experience many noticeable changes, for others, it’s intense, both physically and emotionally.
The first perimenopause sign is often an erratic menstrual cycle. Studies find that, for many women, cycles become more and more unpredictable. The stretch between periods can be longer one month, shorter the next, and flow can be heavier this time around, then suddenly lighter. Your period may go missing entirely for months on end, then come back with a vengeance. Meanwhile, about 75% of women also experience vasomotor symptoms including hot flashes, night sweats, sleep disturbances, mood changes, weight changes, and palpitations during the menopause transition.
What are the Symptoms of Perimenopause and Menopause?
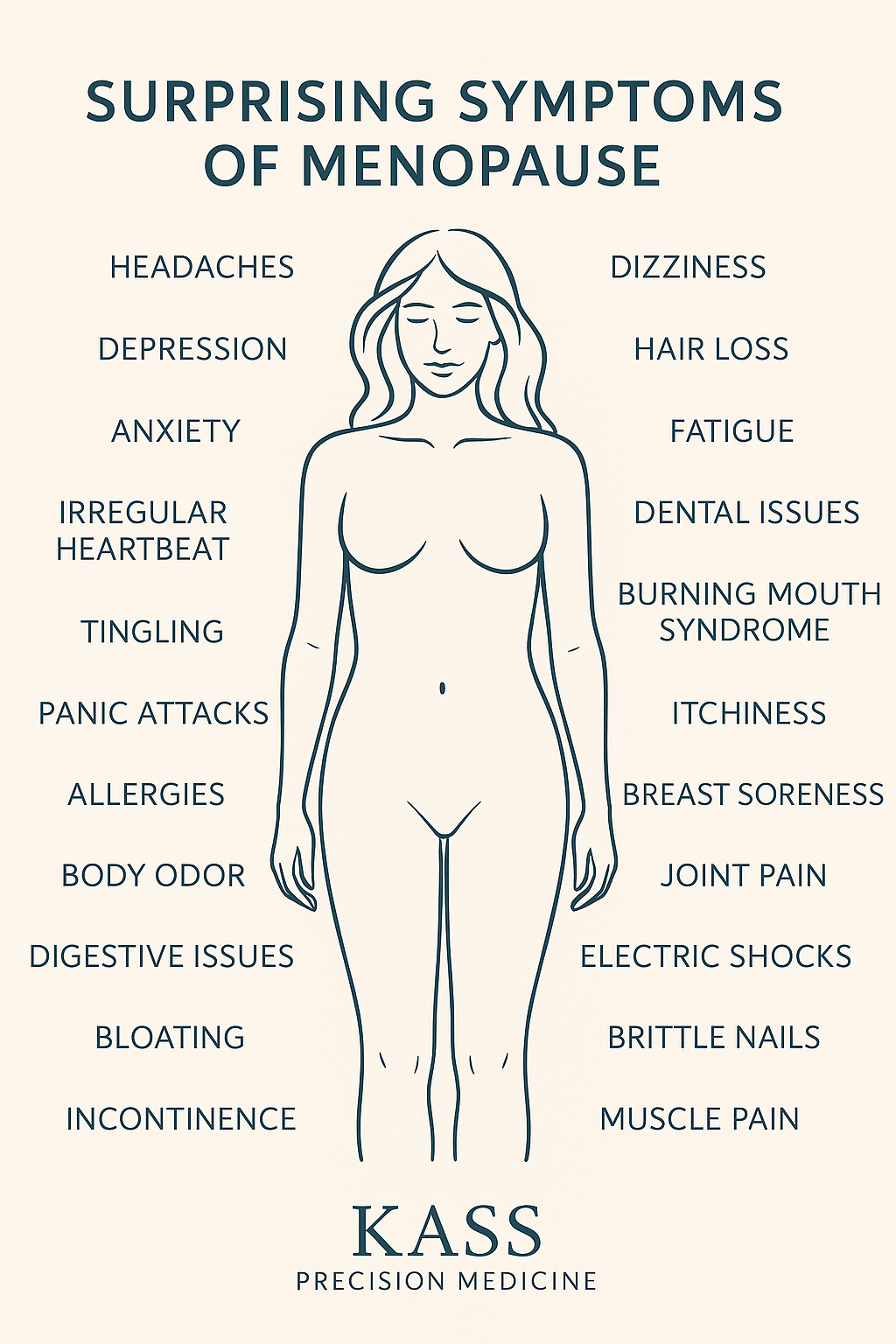
Below is a graphic of symptoms of perimenopause and menopause, many of which you may not have associated with this phase - and neither has your doctor!
If you’re in your 40s and experiencing several of the symptoms below, you may be in perimenopause.
Erratic periods (shorter, longer, or skipping)
Sleep changes
Hot flashes, night sweats
Vaginal Dryness
Mood changes
Sexual function changes
Mental clarity changes
How is perimenopause officially diagnosed?
Unfortunately, perimenopause can be a murky diagnosis. It is diagnosed based on clinical criteria rather than solely on medical tests. Diagnosis is given based on menstrual history, age, and characteristic symptoms.
There are labs that can assist with diagnosis:
FSH (increases)
Estradiol (fluctuates)
Progesterone (decreases more precipitously)
Testosterone (decreases)
Low Inhibin-B (decreases)
AMH (anti-muhlerrian hormone) - an AMH level of less than 10 pg/mL is associated with a high probability of reaching FMP (final menstrual period) within the next 12 months
These tests can assist with diagnosis but are not definitive.
To compound the perimenopause diagnostic problem, women don’t often realize their symptoms are connected to hormonal changes - and neither do their doctors. Symptoms like fatigue, sleep problems, and mood changes are often associated with everyday life stressors or burnout.
Many primary care doctors or OBGYNs are not astute about perimenopause. Symptoms are often overlooked or misidentified. Frequently, birth control is reached for to treat menstrual irregularities. In fact, according to a 2021 survey, 73 percent of women aged 40 to 65 were not currently treating their symptoms.
The big question, then, is, how do you know when you become perimenopausal? Unfortunately, no test can predict when you will start the transition or even fully confirm that you’re in the midst of it. What your physician can do is consider your age, the age at which your mother or sister entered menopause, your health history, all the symptoms you might be experiencing, and order a blood test to measure hormone levels. Remember, though, that your hormones are going up and down a lot during this stage, so a single blood test can be misleading. However, running several tests at different times might provide a clearer picture.
Perimenopause Treatments
Below are the most effective solutions, but remember that some of the symptoms may be associated with other serious conditions and need to be discussed with your doctor.
Medical Interventions
As we discussed above, perimenopause can be a murky diagnosis, and women in their 40s who are not clearly displaying classic menopausal symptoms (i.e., having hot flashes and large periods of time without a menstrual cycle) are often given non-HRT interventions.
Birth control
Oral birth control containing synthetic estrogens and progestins can relieve some perimenopause symptoms like menstrual irregularity, heavy bleeding, menstrual pain, and vasomotor symptoms. Progestin IUDs are often suggested as a way to manage heavy or irregular bleeding.
Off-Label Medications
Antidepressant prescription medications are frequently used off-label for menopause and have shown some efficacy in treating select perimenopausal symptoms. Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and low-dose gabapentin are all shown to improve hot flashes.
Anticholinergic medications like oxybutynin can be prescribed to address hot flashes.
Every medication can have side effects. Specifically, antidepressants and birth control might help with some symptoms but frequently reduce libido and decrease a woman’s ability to achieve orgasm, along with other potential side effects. The cost-benefit of these versus hormone therapy should be discussed with your doctor, ideally one who is educated in all the treatment options.
Hormone Replacement Therapy (HRT)
Sometimes referred to as menopausal hormone therapy or MHT, this is a treatment used during perimenopause and menopause to replenish estrogen and progesterone that naturally decline as your reproductive years wind down.
HRT is the most effective treatment for managing menopause symptoms that result from declining estrogen and progesterone (i.e., hot flashes and vaginal dryness). Standard HRT includes progesterone and estrogen. When a woman with a uterus is prescribed estrogen, she must also take progesterone to protect the uterine lining from becoming too thick (a potential risk factor for endometrial cancer). Also, these medications together generally provide the most thorough symptom relief as they both perform important biologic and neurochemical tasks.
However, if a woman does not have a uterus, it is not standard of care to prescribe progesterone. Standard of care suggests progesterone is only needed to protect the uterine lining. However, for those with no uterus (i.e., had a hysterectomy), certain forms of progesterone may still be recommended off-label to help improve symptoms like sleep issues, night sweats, and mood changes.
While not every woman is a candidate for HRT, most can safely take it, according to the Menopause Society, which is the leading organization in understanding and researching the health of mid-life women. Discuss HRT with your doctor so you can make the right decision for you, your symptoms, and your approach to health.
HRT can frequently help with the following symptoms:
Irregular periods
Breast tenderness
Mood swings
Bloating
Sleep disturbances
Mood changes
Hot flashes and night sweats
Vaginal dryness
Discomfort during sex
Frequent UTIs
Brain fog/poor word recall - mental clarity
Lifestyle Interventions
There is some evidence to suggest that lifestyle factors can mitigate the experience of perimenopause to some degree. Super annoying because perimenopause also contributes to weight gain. That said, studies have shown that carrying extra weight, overconsumption of alcohol, and lack of exercise are all associated with more severe symptoms. For what it’s worth, the following are some lifestyle targets to keep in mind:
Get enough exercise. A general target is 150 minutes a week of some kind of physical activity, ideally combining cardio and strength training.
Perform weight-bearing exercises such as hiking, walking, or strength training.
Eat a whole foods-focused diet centered on vegetables, slow-burn carbs, lean proteins, and healthy fats.
Stress - to the best of your ability, minimize your life stressors because high cortisol can make symptoms worse.
Botanicals - there are a few supplements like black cohosh, Vitex, and maca that can provide modest support.
Perimenopause and Weight Gain
Weight tends to creep up in midlife - women can gain roughly 1-3 pounds per year starting in perimenopause (which can start as early as mid-40s) and continuing through menopause in their early 50s.
Body composition changes more than the scale reveals - perimenopause generally leads to increased fat mass and decreased lean muscle mass during the transition and tends to plateau after a woman stops having menstrual cycles.
Fat shifts to the abdomen (visceral fat) - during the menopause transition, the most pronounced change may not be reflected in the number on the scale, but in the distribution of fat around the midsection (central adiposity). Weight circumference often increases by 4.6 centimeters. These body composition changes are closely tied to hormonal shifts, particularly declining estrogen.
Hormonal Mechanisms of menopausal Weight Gain
Estrogen Decline
Estrogen deficiency leads to up regulation of genes involved in adipogenesis (i.e., new fat generation)
Estrogen deficiency down regulates genes involved in fat oxidation (i.e., impaired ability to utilize fat for energy)
Decreased estrogen also promotes the redistribution of fat - from the periphery to the center (i.e., belly and visceral fat)
Energy expenditure declines, especially fat and energy burned during sleep
Increased vasomotor symptoms leads to worse sleep, mediating more weight gain via cortisol problems
Estrogen deficiency reduces insulin sensitivity, promoting fat storage
Loss of estrogen affects leptin (satiety hormone) sensitivity, increasing appetite
Progesterone Changes
Declining progesterone can increase appetite and cravings
Affects water retention and bloating
Influences cortisol regulation
Sleep & Neuroendocrine Affects
Hot flashes and night sweats disrupt sleep quality
Poor sleep affects hormones regulating hunger (ghrelin and leptin)
Sleep deprivation increases cortisol levels, increasing central weight gain
Body Composition and Muscle
Sarcopenia (loss of lean muscle) - women lose muscle mass during menopause, lowering the base metabolic calorie burn
Increase in visceral and central fat can add to insulin insensitivity, feeding the metabolic problem
Additional Factors
Thyroid problems are more common in menopause
Poor energy during perimenopause and menopause may lead to decreased physical activity
Slower recovery or joint pain may also lead to less physical activity
The combination of these hormonal, metabolic, and lifestyle factors creates a "perfect storm" for weight gain during the menopausal transition, making this period a particularly challenging time for women. KPM understands this issue and is dedicated to helping women successfully reduce weight and improve their quality of life. You can learn more on our Medical Weight Loss and Menopause Medicine pages.
When to See a Doctor for Perimenopause Symptoms
If you are struggling with what you think might be perimenopausal symptoms, do your research and seek out a doctor who specializes in perimenopause/menopause so you can explore the most appropriate treatment option for you.